
The vote was already over. Hands lowered. The screen showed the tally: 8–3. With that, a protection nearly every U.S. newborn had received for 34 years was no longer automatic. As of December 2025, parents—not hospitals—would decide whether low-risk babies get the hepatitis B vaccine at birth.
The change affects 3.6 million newborns a year, immediately. Supporters called it consent restored. Critics saw a hard-won public health victory suddenly put at risk.
Stakes Skyrocket

Hepatitis B is especially dangerous for infants. Nine in ten unvaccinated babies who become infected develop chronic disease, and one in four will eventually die from liver failure or cancer as adults.
Before universal newborn vaccination, about 20,000 U.S. children were infected each year. The birth dose drove pediatric cases down to just 252 chronic infections in 2022. Experts warn that delaying protection—even briefly—reopens a window of preventable risk.
Policy Roots

In 1991, the CDC adopted a universal rule: every U.S. newborn should receive a hepatitis B vaccine within 24 hours of birth, regardless of maternal risk. The logic was simple—screening alone missed cases, and infants were uniquely vulnerable.
The policy proved transformative, becoming a cornerstone of pediatric prevention. For more than three decades, ACIP reinforced this approach. That long-standing consensus now serves as the backdrop for the most consequential reversal in modern U.S. vaccine policy.
Pressures Mount

Over time, resistance to newborn vaccination grew among some parents, fueled by concerns about giving shots on the first day of life. Advocates pointed to Europe, where many countries delay hepatitis B vaccination until two months.
Importantly, no new safety concerns prompted the review. Instead, ACIP reconsidered policy amid broader upheaval at HHS under Secretary Robert F. Kennedy Jr. Persistent gaps in maternal testing—and late household exposures—remained unresolved as momentum for change built.
ACIP Votes to Change Policy

On December 5, 2025, ACIP voted 8–3 to end universal hepatitis B vaccination at birth for infants born to mothers who test negative for the virus. The committee adopted a shared clinical decision-making model, allowing parents to opt in or delay.
Acting CDC Director Jim O’Neill approved the recommendation on December 16, making it official policy. For the first time since 1991, protection at birth would no longer be automatic for most newborns.
U.S. Impact Hits

The shift affects millions of low-risk newborns each year. Infants born to mothers who are hepatitis B–positive—or whose status is unknown—will still receive the vaccine within 12 hours, plus immunoglobulin.
Insurance coverage remains unchanged through programs like Vaccines for Children and Medicaid. But hospitals nationwide now face diverging practices. Public health officials are watching closely: will vaccination rates hold, or slowly erode as decisions shift from protocol to conversation?
Parents Empowered

“This restores the balance of informed consent,” Acting CDC Director Jim O’Neill said, arguing that most low-risk newborns face minimal exposure. Under the new guidance, families are encouraged to consider household contacts, travel, and caregiving environments when deciding.
If delayed, the first dose is recommended no earlier than two months, leaving a temporary protection gap. Supporters see autonomy. Critics worry parents are being asked to assess risks that are often invisible and unknowable.
Pediatrics Pushes Back

The American Academy of Pediatrics (AAP) forcefully rejected the new guidance, reaffirming its recommendation that all newborns be vaccinated within 24 hours. Major hospitals—including Lurie Children’s Hospital of Chicago—announced they will continue universal dosing.
Several state health departments, including New York and Connecticut, aligned with pediatricians rather than the CDC. The result is a fractured landscape, with clinicians caught between federal policy and longstanding professional standards.
A Public Health Success Story

Since 1991, universal newborn vaccination helped drive a 93% drop in hepatitis B infections overall and a 99% reduction in chronic pediatric cases. Childhood coverage reached 91.4% by age two, one of the CDC’s most cited successes.
ACIP members acknowledged these gains—but argued that declining disease burden now stems more from screening and surveillance. Critics counter that success is precisely why the policy should remain untouched.
RFK Jr.’s ACIP Overhaul
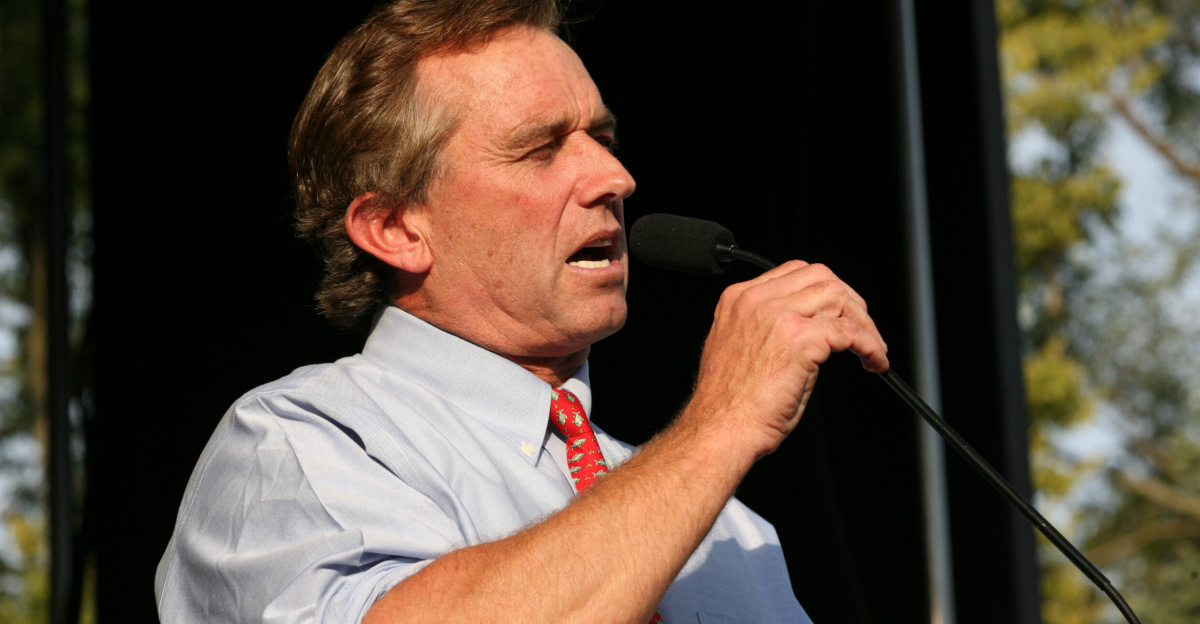
The vote followed an unprecedented shake-up. In June 2025, HHS Secretary Robert F. Kennedy Jr. fired all 17 ACIP members, replacing them with a hand-picked panel.
Kennedy, a longtime vaccine skeptic and founder of Children’s Health Defense, denied ideological motives. Critics disagreed, calling the hepatitis B decision the first clear policy consequence. While vaccine injury liability rules remain unchanged, the committee’s credibility—and independence—came under intense scrutiny.
Experts Clash

Opposition was swift and blunt. Senator Bill Cassidy, a physician, warned the move would “make America sicker.” Pediatric leaders cited past patients who died after early infection.
Dissenting ACIP members defended the decision as evidence-based, emphasizing safety data and parental choice. Congressional hearings grew heated as both sides accused the other of politicizing science. What had once been technical guidance became a national argument over risk, trust, and authority.
Leadership Shift

The policy change reflects a broader realignment inside federal health agencies. With RFK Jr. at HHS and Jim O’Neill as Acting CDC Director, ACIP’s priorities shifted rapidly.
New chair Dr. Kirk Milhoan promoted enhanced post-vaccination blood testing, despite limited supporting data. Leading vaccine experts Paul Offit and Peter Hotez refused to participate, calling the committee illegitimate. The center of vaccine decision-making moved—abruptly and controversially.
Hospitals Hold Firm

Many pediatric systems are staying the course. “We cannot predict exposure,” said Lurie Children’s infectious disease chief Dr. Ravi Jhaveri. Children’s Hospital Atlanta echoed the stance, citing decades of evidence.
Some states issued standing orders to preserve access regardless of CDC guidance. For frontline clinicians, continuity matters more than policy shifts. In practice, newborn care may depend less on federal recommendations than on institutional resolve.
Skeptics Warn of Consequences

Modeling presented to ACIP suggested that delaying vaccination could result in 1,400 new chronic infections in the first year alone, eventually leading to hundreds of liver cancer cases.
The committee acknowledged it lacks data on how much protection a single birth dose provides—but critics argue that uncertainty cuts both ways. The AAP boycotts subsequent meetings, calling the decision “dangerous.” For opponents, the risk of resurgence outweighs any theoretical benefit.
The Road Ahead

Will vaccination rates fall below 91%, or will parents continue opting in? ACIP is now reviewing the entire childhood immunization schedule, signaling more potential changes.
A separate vote narrowly endorsed expanded blood testing after the first dose. Insurers still cover all hepatitis B vaccines, but parents may face confusion at delivery. Trust—once assumed—now requires explanation.
A Political Battleground

The hepatitis B decision has become a proxy for a larger fight over vaccines. Lawmakers like Sen. Cassidy urged the CDC to reverse course. States such as Illinois and Connecticut openly defied federal guidance.
What was once a unified system—CDC, ACIP, AAP aligned—now operates at cross-purposes. Public health, long shielded from partisan conflict, is increasingly shaped by ideology, appointments, and power struggles at the highest levels.
Global Contrast

By ending universal newborn vaccination, the U.S. moves closer to much of Europe, where low-risk infants typically wait until two months. Yet 116 of 194 WHO member states still recommend a birth dose.
The U.S. has large immigrant populations from high-endemic regions, complicating risk assessment. ACIP cited international norms—but critics argue America’s demographics and health system make direct comparisons misleading.
Legal Protections Remain

Despite the controversy, liability rules did not change. Hepatitis B vaccines remain covered under the National Vaccine Injury Compensation Program (VICP).
Pediatricians following AAP guidance retain legal protection, according to health law experts. Still, RFK Jr. warned providers of risks in diverging from CDC recommendations. If infections rise, lawsuits may follow—not over injury from vaccines, but over missed opportunities to prevent disease.
Ethics in Transition

Shared decision-making reframes vaccination as a personal choice rather than a default safeguard. Proponents argue this respects parental autonomy.
Pediatricians counter that true consent requires understanding invisible risks—like asymptomatic carriers, faulty tests, and a virus that survives up to seven days on surfaces. The ethical balance has shifted: from population-level prevention to individualized judgment.
What This Moment Signals

This reversal tests the resilience of U.S. vaccine confidence after decades of success. A policy that helped eliminate 20,000 childhood infections a year is now optional.
As ACIP considers further changes, the emphasis tilts toward choice over uniform protection. Whether this marks a careful recalibration—or the start of broader erosion—will depend on what happens next, in hospitals, delivery rooms, and the quiet decisions made in a newborn’s first hours of life.
Sources:
Centers for Disease Control and Prevention (CDC): CDC Releases Updated Hepatitis B Immunization Recommendations (December 16, 2025)
American Academy of Pediatrics (AAP): AAP Reaffirms Recommendation for Hepatitis B Vaccine at Birth Despite New CDC Guidance (December 16, 2025)
Pharmacy Times: ACIP Votes to End Universal Hepatitis B Vaccination Recommendation for Infants (December 10, 2025)
BBC News: RFK Jr Fires Entire US Vaccine Committee (June 9, 2025)
STAT News: CDC Vaccine Panel Poised to Recommend Changing Hepatitis B Birth Dose (December 4, 2025)