
State officials began quietly removing providers from Minnesota’s Medicaid system—hundreds at a time—triggering sudden changes inside one of the state’s largest public health networks.
By October, about 800 providers had been stripped from the rolls after going more than a year without billing for care. For patients checking directories and clinics reviewing enrollment lists, the shift felt immediate. And officials made one thing clear: this was only the first round.
Fraud Shadows Grow
Minnesota’s action did not happen in isolation. The state has faced repeated fraud scandals across public programs, most notably the massive Feeding Our Future case.
Lawmakers and investigators have argued that weak oversight allowed fraudulent or inactive entities to linger for years. As public trust eroded, pressure mounted for decisive action. Medicaid, one of the largest and most complex programs, became the next focal point in the state’s broader integrity crackdown.
Walz Steps In

In response, Governor Tim Walz issued Executive Order 25-10, directing the Minnesota Department of Human Services to strengthen Medicaid program integrity.
The order emphasized closing long-standing oversight gaps and removing providers that no longer actively served patients. State leaders framed the effort as overdue cleanup rather than a policy shift. Still, the scale and speed of the directive signaled a more aggressive posture moving forward.
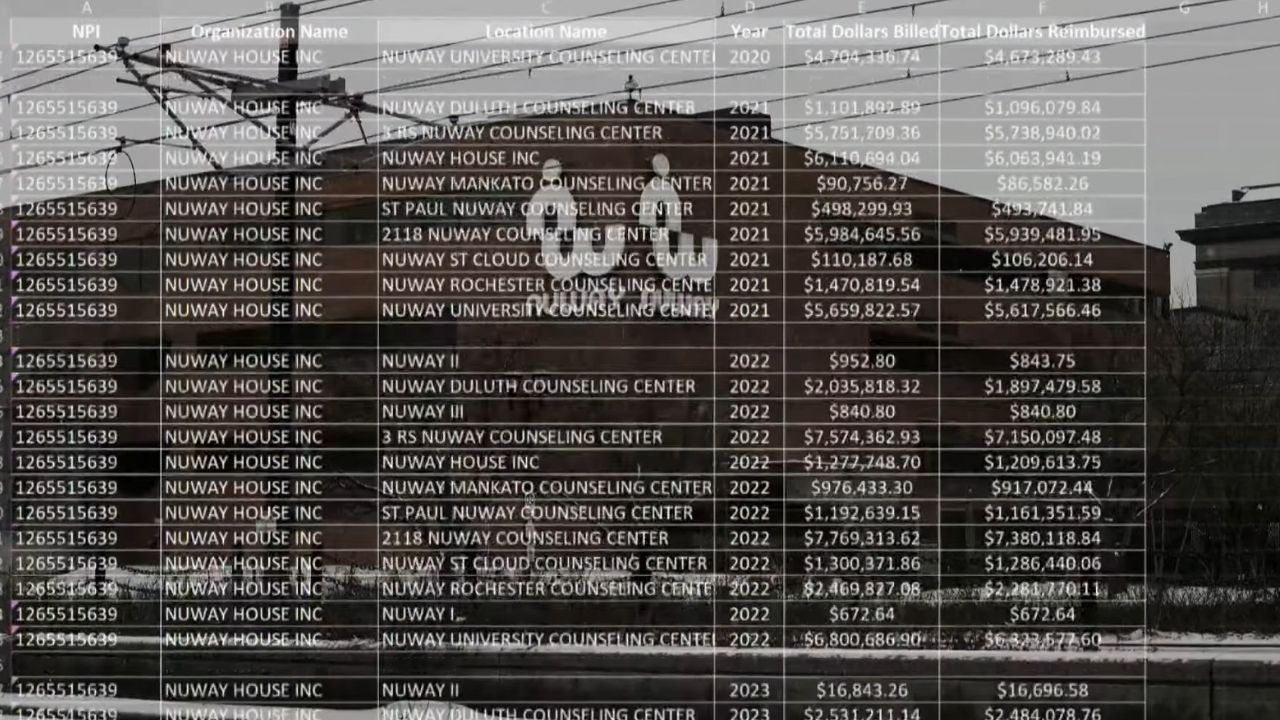
Billing Red Flags
Under the new approach, DHS identified high-risk Medicaid services for intensified scrutiny, including areas historically vulnerable to abuse. Providers showing irregular billing patterns or missing documentation became subject to audits and payment reviews.
In some cases, payments were paused while claims were examined. Officials stressed that the goal was prevention, not punishment, but the message was clear: enrollment alone would no longer shield inactive or questionable providers from oversight.
800 Providers Removed

By October 2025, Minnesota Department of Human Services confirmed the disenrollment of roughly 800 Medicaid providers in what it described as the first round of removals. Each provider had gone more than 12 months without submitting a Medicaid claim.
State officials emphasized that these providers were inactive, not necessarily accused of fraud. Additional rounds of disenrollment were expected as reviews continued.
1.3 Million on Alert
The removals immediately raised concerns for the 1.3 million Minnesotans who rely on publicly funded health care. Even if many providers were inactive, their removal introduced uncertainty into an already strained system.
Patients were urged to review provider directories and confirm their care arrangements. In rural and underserved areas, where provider options are limited, even small network changes can create outsized disruptions.
Real Lives, Real Confusion
For patients, the policy shift translated into confusion and anxiety. DHS acknowledged that some enrollees may need to find new providers or confirm whether their current providers remained enrolled.
Advocacy groups warned that individuals with disabilities, chronic illnesses, or complex care needs could be most affected. While officials emphasized that care continuity remained a priority, the human impact of rapid system changes became increasingly visible.
Lawmakers Demand Answers

Federal scrutiny soon followed. Minnesota’s congressional delegation called for deeper investigations into how inactive or fraudulent providers remained enrolled for so long.
Lawmakers pointed to the scale of federal Medicaid funding flowing through the state and questioned whether existing controls were sufficient. With national attention focused on health care fraud enforcement, Minnesota’s Medicaid system became part of a much larger accountability debate.
A Pattern Years in the Making

Investigations and reporting have revealed that Medicaid vulnerabilities in Minnesota stretch back more than a decade. Previous cases involved daycare services, community supports, and home care billing schemes. Despite periodic reforms, new fraud patterns continued to emerge.
State leaders have argued that the current purge reflects lessons learned from those failures. Critics counter that lasting reform requires more than periodic cleanups.
The “Inactive” Network
Officials stressed that many removed providers were effectively dormant, sometimes existing only on paper. Some had not served patients in years but remained eligible to bill Medicaid. Cleaning out these inactive records was framed as basic system maintenance.
Still, the sheer number of removals raised questions about how long outdated enrollments persisted and how accurately Medicaid provider networks reflected real-world access.
Provider Backlash
Not all providers accepted the removals quietly. Some argued that extended inactivity resulted from staffing shortages, administrative delays, or temporary closures rather than abandonment of Medicaid.
Smaller practices, in particular, warned that rigid billing thresholds could unfairly penalize legitimate providers. DHS maintained that appeal processes were available, but frustration grew as providers navigated reinstatement pathways.
Leadership and Oversight Reset

Under interim leadership, DHS pledged a more systematic approach to fraud prevention and program monitoring. New oversight mechanisms, including expanded audits and interagency coordination, were introduced.
Officials framed the changes as essential to restoring public trust. Whether these leadership and structural changes will produce lasting improvements remains an open question for both lawmakers and beneficiaries.
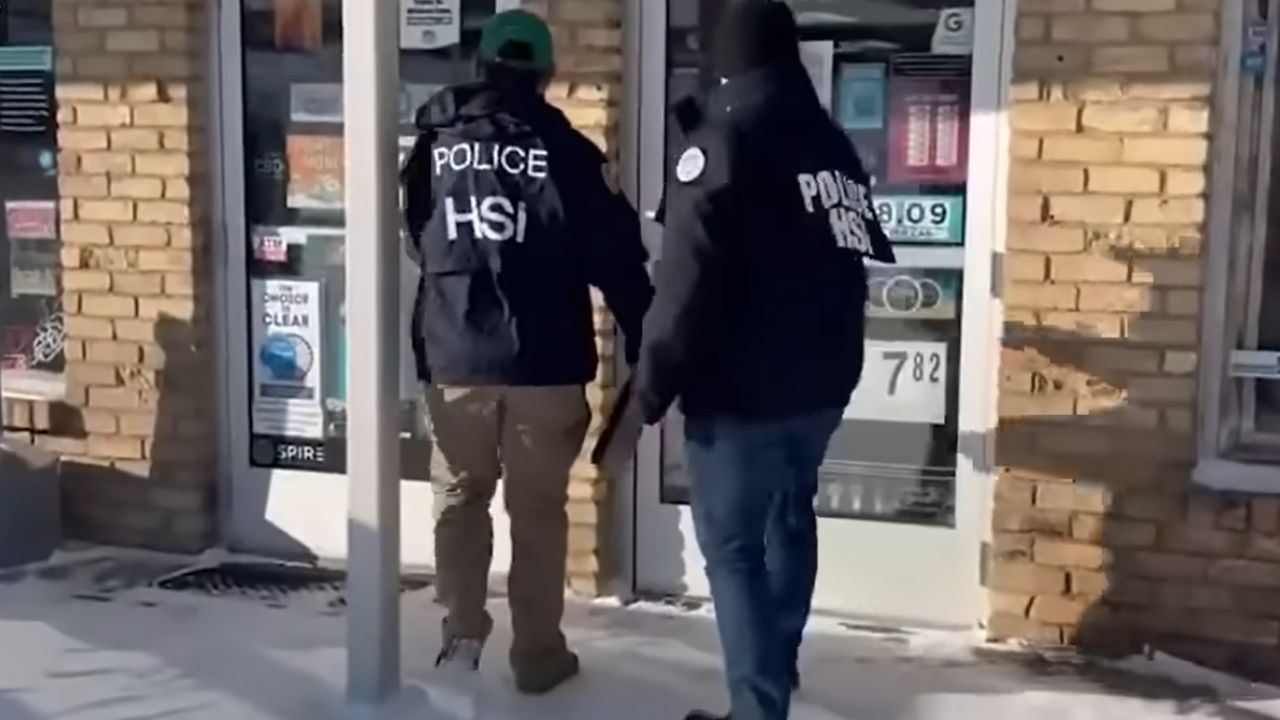
A National Enforcement Backdrop
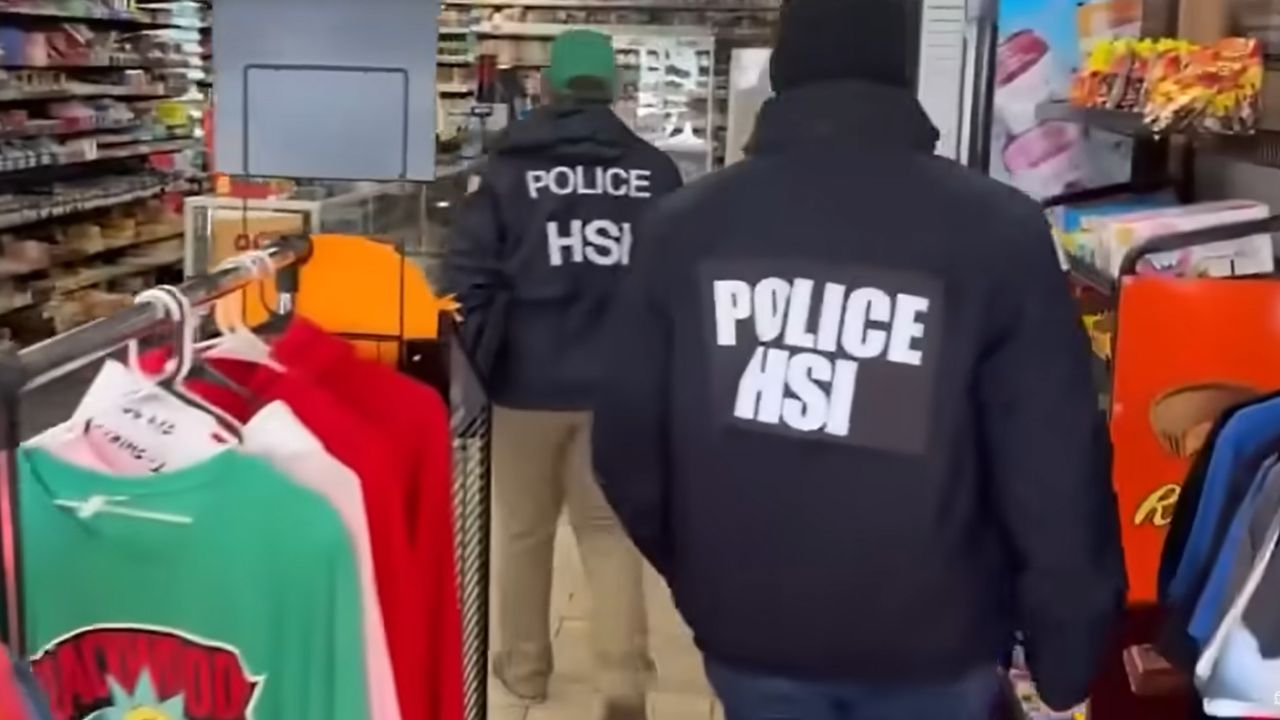
Minnesota’s actions coincided with heightened federal enforcement nationwide. In 2025, the U.S. Department of Justice announced one of its largest coordinated health care fraud takedowns, charging hundreds of defendants across dozens of federal districts.
State officials cited this broader context as evidence that Medicaid fraud is not a theoretical issue, but an active, nationwide challenge demanding constant vigilance.
Funding Pressures Ahead
The crackdown unfolds against a difficult fiscal backdrop. Federal projections from the Congressional Budget Office estimate more than $1 trillion in Medicaid cuts by 2034, potentially leaving millions uninsured nationwide.
At the same time, policy shifts under the Donald Trump administration proposed further reductions. For states, safeguarding every Medicaid dollar has become increasingly urgent.
Care at a Crossroads
Minnesota’s Medicaid purge marks a decisive moment. State leaders insist that removing inactive providers strengthens program integrity and protects vulnerable residents. Critics worry about access gaps and unintended consequences.
With more dis-enrollments possible and federal scrutiny ongoing, the stakes are high. For the 1.3 million Minnesotans who depend on Medicaid, the challenge now is ensuring that accountability reforms do not come at the cost of timely, reliable care.
Sources:
“Executive Order 25-10: Combatting Fraud in State Programs.” Office of Governor Tim Walz, Minnesota, 16 Sept 2025.
“DHS Drops Hundreds of Minnesota Medicaid Providers in Steps to Combat Fraud.” KSTP News, 16 Oct 2025.
“National Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Intended Loss.” U.S. Department of Justice, 29 June 2025.
“How Fraud Swamped Minnesota’s Social Services System.” The New York Times, 29 Nov 2025.